- Platform is powered by Cedar's innovative Payer Intelligence Layer, and is a key component of Highmark Health's Living Health care model
- Delivers real-time access to medical bills, benefits coverage verification, deductible status, health savings account balances and more
During a single healthcare encounter, a typical consumer may have multiple, disconnected interactions with their provider and payer about the financial aspects of their visit. For example, consumers looking to pay a bill, check their deductible progress or verify their health benefit account balance might have to utilize multiple communications methods, such as phone calls, apps or provider- and insurer-affiliated web portals.
This lack of alignment leads to frustration and confusion for consumers, resulting in missed payments, overspending, administrative waste and money left on the table for consumers, who may be unaware of their available spending account funds. Not only do U.S. consumers spend 12 million hours a week on the phone with health insurers, but more than one-third of consumers have been sent to debt collections because of a billing issue between their healthcare provider and health insurer.
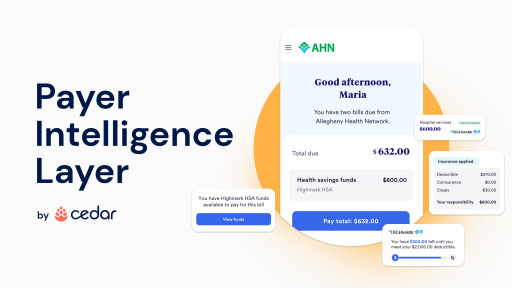
To address the systemic challenges consumers face when paying for healthcare, Cedar, an enterprise healthcare engagement platform that improves the end-to-end consumer financial journey, has developed the Payer Intelligence Layer. With the Payer Intelligence Layer, Cedar can now integrate data from health insurers and healthcare providers to help create a single source of information for consumers managing medical bills. A game-changer for the healthcare industry, Pittsburgh-based Highmark Inc. and Allegheny Health Network (AHN) will be the first to launch the new technology for services provided to Highmark Inc. members at AHN wholly owned providers and facilities.
"For too long, payer and provider misalignment has led to a poor experience and lack of clarity for consumers managing healthcare bills — this is a system problem, requiring a system solution," said Seth Cohen, president of Cedar. "When each party plays a separate role, neither can fix the experience alone. But by bringing both sides together, we can create the best possible experience, reducing billing friction for consumers while delivering more efficient operations for payers and providers."
Initially available with Cedar Pay, the company's billing and payment solution, the Payer Intelligence Layer enables consumers to access insurance explanation of benefits, real-time deductible status and health benefit accounts in the same place where they view and resolve medical bills — using a single, intuitive interface. Unlike other patient billing solutions, Cedar ensures consumers have the most up-to-date benefits information at their fingertips by directly integrating with health insurers as well as banks, which are responsible for administering health savings accounts, flexible spending accounts and health reimbursement accounts.
"Healthcare billing can be fragmented, cumbersome and overwhelming to navigate," said Neil Kulkarni, vice president, Customer and Clinician Experience Solutions at Highmark Health. "Consumers want clear, easy-to-understand bills for their care and a simple way to pay — with their spending account information available across all channels. As part of Highmark Health's Living Health model designed to deliver a blended and seamless health care experience, our collaboration with Cedar will help us to meet those customer expectations," he said.
"The financial experience in healthcare is a real pain point for most consumers, and for most care providers. The issues associated with healthcare billing can only be resolved if all major players come together and collaborate for the benefit of consumers," said James Rohrbaugh, chief financial officer and treasurer at Allegheny Health Network. "Our work with Cedar will be important in driving real progress in this area, helping our patients and members with an intuitive experience that fosters a sense of control and understanding about their financial responsibility."
AHN and Highmark are collaborating with Cedar in distinct but integrated ways. Patients who visit AHN providers and facilities will experience the new and enhanced billing, statement and call center process, and simplified access to flexible payment options, all driven by the Cedar Pay platform. For AHN patients who are also enrolled as Highmark members, the enhancements multiply. Beginning at the end of October, the nearly 300,000 members visiting AHN providers will now have the added benefit of having their insurance information incorporated directly into a single billing statement. Members will see how their benefits have been applied, available health spending account funds and their progress towards their deductible and out-of-pocket limits — both when paying AHN bills online, and on the mailed paper statements.
"We're excited to be launching with healthcare industry leaders Highmark Health and Allegheny Health Network to solve this persistent problem," added Cohen, Cedar's president. "But this is only the beginning: Cedar is continuing to explore more ways of leveraging payer data and new integrations to enrich the end-to-end healthcare experience for today's consumers."
About Cedar
Cedar is committed to improving the healthcare financial experience for all. With an innovative platform that connects providers and payers, Cedar empowers healthcare consumers with an optimized journey — all powered by data science and interactive design. For Cedar clients, this leads to increased payments, more efficient operations and greater consumer loyalty. To learn more about why leading U.S. healthcare organizations trust Cedar to manage the end-to-end consumer experience from pre-registration to post-visit billing, visit www.cedar.com and join us on LinkedIn, Twitter, Facebook and YouTube.
About Highmark Health
Highmark Health, a Pittsburgh, Pennsylvania-based enterprise that employs more than 37,000 people who serve millions of Americans across the country, is the parent company of Highmark Inc., Allegheny Health Network, enGen, Helion, and Lumevity. Highmark Inc. and its subsidiaries and affiliates provide health insurance to more than six million members in Pennsylvania, West Virginia, Delaware, and New York, as well as dental insurance, and related health products through a national network of diversified businesses. Allegheny Health Network is an integrated delivery network in western Pennsylvania comprised of 14 hospitals, more than 2,600 affiliated physicians, ambulatory surgery centers, an employed physician organization, home and community-based health services, a research institute, a group purchasing organization, and health and wellness pavilions. enGen is focused on meeting the information technology platform and other business needs of the Highmark Health enterprise as well as unaffiliated health insurance plans by providing proven business processes, expert knowledge, and integrated cloud-based platforms. Helion works with payers to cultivate high-performing networks while empowering providers to operate at their best. Lumevity helps companies transform in ways that drive direct financial benefits while improving quality and increasing employee engagement. To learn more, visit www.highmarkhealth.org.
About Allegheny Health Network
Allegheny Health Network (AHN.org), a Highmark Health company, is an integrated health care delivery system serving the greater Western Pennsylvania region. The network is composed of 14 hospitals, ambulatory surgery centers, Health + Wellness Pavilions, an employed physician organization, home- and community-based health services, a research institute, and a group purchasing organization. AHN provides patients with access to a complete spectrum of advanced medical services, including nationally recognized programs for primary and emergency care, cardiovascular disease, cancer care, orthopedic surgery, neurology and neurosurgery, women's health, diabetes and more. AHN employs approximately 21,000 people, has more than 2,600 physicians on its medical staff, and serves as a clinical campus for Drexel University College of Medicine and the Lake Erie College of Osteopathic Medicine.
Contact Information:
Rachel Borowski
Highmark Health
[email protected]
Bill Toland
Allegheny Health Network
[email protected]
Jenny Fiegoli
Cedar
[email protected]
Press Release Service by Newswire.com
Original Source: Cedar's Integrated Payer-Provider Patient Billing Platform Introduced to Highmark Inc. and Allegheny Health Network Customers